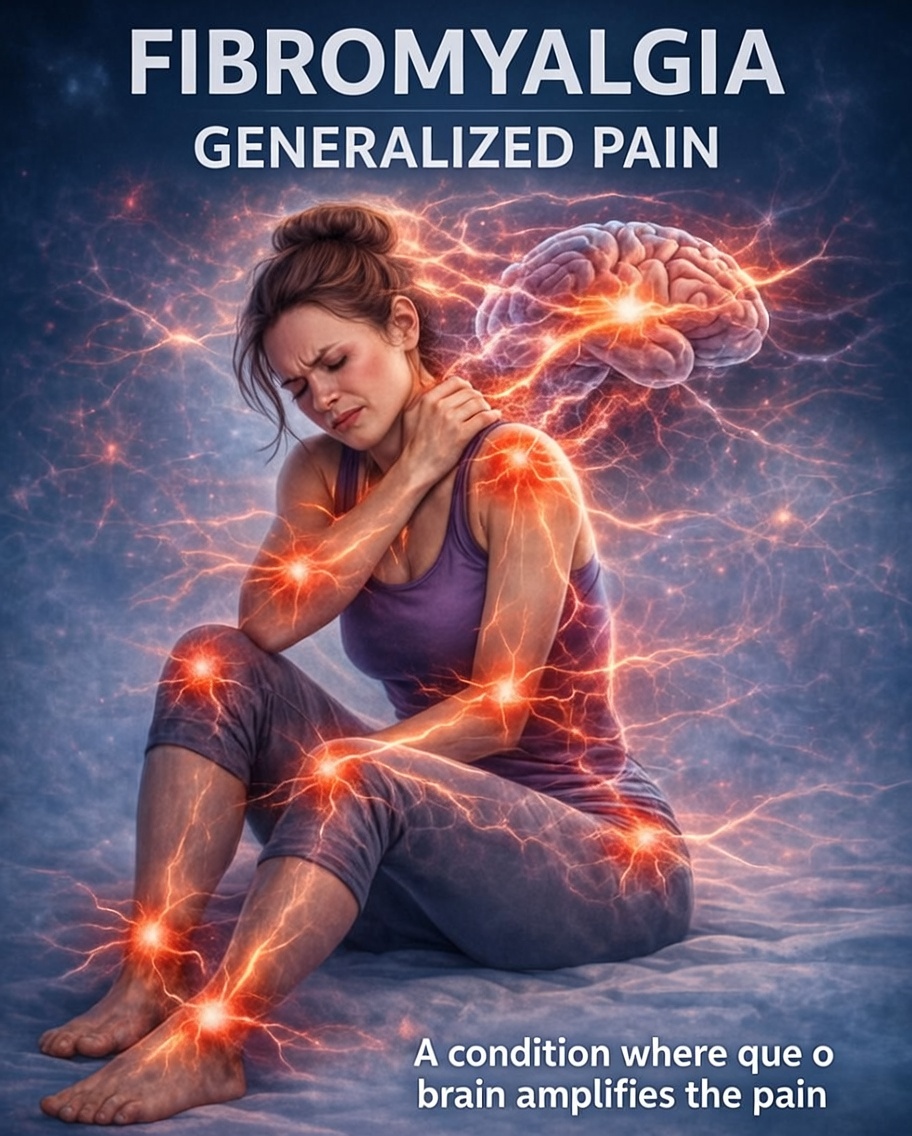
Fibromyalgia is a chronic neurological condition characterized by generalized pain, heightened sensitivity, and persistent discomfort that affects the entire body. Unlike pain caused by injury or inflammation, fibromyalgia pain originates from altered pain processing in the central nervous system, where the brain amplifies normal sensory signals and interprets them as intense pain.
This condition impacts millions of people worldwide and remains widely misunderstood. The pain is real, debilitating, and life-altering—even when medical tests appear normal. Understanding how fibromyalgia causes generalized pain is essential for awareness, validation, and effective symptom management.
What Is Fibromyalgia?
Fibromyalgia is a chronic pain disorder marked by widespread musculoskeletal pain, fatigue, sleep disturbances, and cognitive difficulties. It is classified as a central sensitization syndrome, meaning the brain and spinal cord become overly sensitive to pain signals.
Rather than a problem in muscles or joints, fibromyalgia involves a dysfunction in how the nervous system processes pain. Everyday sensations—pressure, temperature changes, light touch—may be perceived as painful or overwhelming.
Primary keywords: fibromyalgia, fibromyalgia pain, chronic pain condition
Secondary keywords: fibromyalgia symptoms, neurological disorder, chronic illness
Understanding Generalized Pain in Fibromyalgia
Generalized pain is the hallmark symptom of fibromyalgia. It does not stay in one location or follow a predictable pattern. Instead, it spreads across multiple regions of the body and may shift from day to day.
People with fibromyalgia often describe pain as:
-
Deep aching
-
Burning sensations
-
Stiffness
-
Throbbing
-
Sharp or stabbing pain
-
Extreme tenderness to touch
This pain is persistent, often present for months or years, and cannot be explained by structural damage or inflammation.
How the Brain Amplifies Pain Signals
In fibromyalgia, the brain’s pain “volume control” is turned up too high.
Normally, the nervous system has mechanisms that filter, inhibit, and regulate pain. In fibromyalgia, these mechanisms function inadequately. The brain:
-
Overreacts to mild stimuli
-
Fails to dampen pain signals
-
Remains in a state of heightened alert
This phenomenon is known as central sensitization, and it explains why fibromyalgia pain feels intense, widespread, and exhausting.
SEO keywords: central sensitization, pain amplification, nervous system dysfunction
Why Fibromyalgia Pain Is Not Caused by Inflammation
One of the most common misconceptions is that fibromyalgia is an inflammatory or autoimmune disease. While inflammation can coexist with fibromyalgia, it is not the root cause of the pain.
Medical imaging and blood tests often return normal results, leading to frustration and disbelief. However, fibromyalgia pain is:
-
Neurological, not structural
-
Functional, not visible on scans
-
Real, even without tissue damage
This absence of visible markers does not invalidate the condition—it highlights the complexity of the nervous system.
Diffuse Pain Without a Fixed Point of Origin
Unlike localized pain, fibromyalgia pain often lacks a clear source. There is no single injured muscle or joint to treat. Instead, pain:
-
Moves throughout the body
-
Appears symmetrically on both sides
-
Affects muscles, tendons, and soft tissues
This diffuse nature contributes to feelings of helplessness and confusion, especially early in diagnosis.
The Role of the Central Nervous System
The central nervous system (CNS) plays a central role in fibromyalgia. Research shows abnormalities in:
-
Pain neurotransmitters
-
Sensory signal processing
-
Stress response pathways
The CNS remains in a state of hyperarousal, making the body react as though it is constantly under threat. Over time, this leads to chronic pain, fatigue, and sensory overload.
Fibromyalgia Pain and Sensitivity to Touch
Many people with fibromyalgia experience allodynia, a condition where non-painful stimuli cause pain. Simple actions such as:
-
Wearing tight clothing
-
Being lightly touched
-
Sitting for long periods
can trigger discomfort or pain. This heightened sensitivity reinforces the idea that fibromyalgia is not “imagined” but rooted in neurological changes.
Pain Types Commonly Experienced in Fibromyalgia
Fibromyalgia pain is not uniform. It can present in different forms, including:
Burning Pain
Often described as nerve-like or electric, this sensation may worsen at night.
Heavy or Crushing Pain
A feeling of weight pressing on the body, especially in the chest or limbs.
Stiffness and Morning Pain
Many people wake up feeling rigid, sore, and unrested.
Migratory Pain
Pain that shifts location throughout the day or week.
Why Fibromyalgia Affects the Entire Body
Because the brain processes pain signals globally, fibromyalgia pain is not limited to one system. It affects:
-
Muscles
-
Skin
-
Joints
-
Internal organs
This whole-body involvement explains why fibromyalgia often overlaps with other conditions such as irritable bowel syndrome, migraines, and chronic fatigue syndrome.
The Impact of Chronic Pain on Daily Functioning
Living with constant pain changes every aspect of life. Fibromyalgia pain interferes with:
-
Physical mobility
-
Work productivity
-
Emotional health
-
Social relationships
Simple tasks can become overwhelming when pain is relentless and unpredictable.
Fibromyalgia Pain and Sleep Disturbances
Pain and sleep are deeply interconnected. In fibromyalgia:
-
Pain disrupts sleep cycles
-
Non-restorative sleep increases pain sensitivity
-
Fatigue amplifies pain perception
This creates a vicious cycle where poor sleep worsens pain, and pain prevents quality sleep.
SEO keywords: fibromyalgia fatigue, sleep problems, non-restorative sleep
Emotional and Cognitive Effects of Persistent Pain
Chronic generalized pain places a heavy burden on mental health. Many individuals experience:
-
Anxiety
-
Depression
-
Mood changes
-
Cognitive difficulties (“fibro fog”)
These effects are not signs of weakness—they are natural responses to prolonged neurological stress.
Why Fibromyalgia Pain Is Often Dismissed
Despite growing research, fibromyalgia is still frequently misunderstood. Reasons include:
-
Lack of visible damage
-
Variable symptoms
-
Outdated beliefs about pain
This dismissal can be more damaging than the pain itself, leading to delayed diagnosis and inadequate care.
Fibromyalgia as a Recognized Neurological Condition
Today, fibromyalgia is recognized by major health organizations as a legitimate neurological disorder. Advances in brain imaging and pain science confirm altered pain processing pathways in people with fibromyalgia.
Recognition matters. It validates patient experiences and supports access to appropriate treatment.
Managing Generalized Pain in Fibromyalgia
While there is no cure, fibromyalgia pain can be managed through a multidisciplinary approach, including:
-
Pain-modulating medications
-
Gentle physical activity
-
Cognitive behavioral strategies
-
Stress reduction techniques
-
Sleep optimization
Treatment focuses on calming the nervous system rather than treating inflammation or injury.
The Importance of Validation and Awareness
Believing people with fibromyalgia is crucial. Validation:
-
Reduces emotional distress
-
Improves treatment outcomes
-
Encourages self-advocacy
Awareness helps dismantle stigma and promotes earlier diagnosis and better support.
Living With Fibromyalgia: Quality of Life Matters
Fibromyalgia may be chronic, but life does not end with diagnosis. With proper understanding, support, and self-management strategies, many people learn to adapt, pace themselves, and reclaim meaningful parts of life.
Pain does not define a person—but acknowledging it is essential for healing.
Final Thoughts: Fibromyalgia Pain Is Real
Fibromyalgia generalized pain is not imaginary, exaggerated, or psychological. It is the result of real neurological changes that alter how the brain perceives pain.
Understanding this condition helps replace doubt with compassion and misinformation with science. Fibromyalgia is complex, real, and deserving of recognition, research, and respect.